Patients who receive chemotherapy and radiation after surgery for gastric cancer appear to have better survival rates than those who had surgery followed by only chemotherapy, according to results of a look-back study of more than 500 people by Johns Hopkins scientists.
The combination of post-operative chemotherapy and radiation, or chemoradiation, resulted in survival for an average of 46.7 months after treatment, compared to 20.9 months among those who received chemotherapy only after surgery. Five years after treatment, 46.9 percent of chemoradiation-plus-surgery patients were still living, while 24.9 percent of chemotherapy-plus-surgery patients survived.
Chemoradiation also improved patients’ recurrence-free survival, to an average of 35.6 months, compared with 16.6 months among those who received chemotherapy alone.
The addition of radiation especially improved survival rates among gastric cancer patients whose cancers had spread to lymph nodes in the immediate region of the stomach, says Timothy Pawlik, M.D., M.P.H., Ph.D., professor of surgery at the Johns Hopkins University School of Medicine and member of the Johns Hopkins Kimmel Cancer Center.
Pawlik says the role of radiation therapy in treating gastric cancer has been understudied, “but these data would suggest that radiation therapy would benefit patients, in particular those patients who had disease that has spread to lymph nodes.”
Although rates of gastric cancer have dropped in recent years in the United States, it is still the fourth most common cancer and the second-leading cause of cancer deaths worldwide.
The study results, described in the Annals of Surgical Oncology, is a so-called retrospective one, looking at the records of 505 gastric cancer patients treated between 2000 and 2012. Retrospective studies come with a certain amount of limitation and bias, Pawlik says, because researchers can only analyze how therapy was carried out and can’t control which patients received which treatments.
Pawlik and his colleagues attempted to remove some of that bias in their study with a statistical fix. Using information on the patients’ ages, tumor sizes and other factors collected from the multi-institutional U.S. Gastric Cancer Collaborative database, the researchers were able to build a score that measured how likely it would be for a patient to receive chemoradiation along with surgery. Within groups of patients with similar scores, they were able to compare the outcomes between those who did get chemoradiation and those who had chemotherapy only.
This “fancy matching” helps get rid of some but not all of the bias in a retrospective study, says Pawlik. “It is possible that patients who got radiation therapy were younger, healthier, and could more easily tolerate radiation therapy, which factored into longer survival.”
Chemoradiation therapy also has improved over the past decade, making it an important tool to consider when treating gastric cancer, says Joseph Herman, M.D., director of clinical research in the Department of Radiation Oncology and Molecular Radiation Sciences at Johns Hopkins. “Some patients will benefit more from chemoradiation, and these large studies can give us more insight into who these patients might be.”
Other researchers involved in the study include Aslam Ejaz, Gaya Spolverato and Yuhree Kim of the Johns Hopkins University School of Medicine; Malcolm H. Squires and Shishir K. Maithel of Emory University; George Poultsides and David J. Worhunskyof Stanford University; Ryan Fields and Linda X. Jin of Washington University in St. Louis; Mark Bloomston, Carl Schmidt and Neil Saunders of The Ohio State University; Sharon M. Weber, Alexandra W. Acher and Clifford S. Cho of the University of Wisconsin; and Konstantinos Votanopoulos and Douglas Swords of Wake Forest University.
Ejaz was supported in part by the Eleanor B. Pillsbury Foundation for Surgical Research
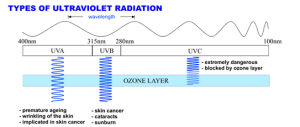
 A substantial gap exists between patient expectations and current practices for providing information about medical imaging tests that use radiation, according to a new study published online in the journal Radiology. Researchers said the findings highlight a need for better communication as medicine enters an era of patient-centered care.In recent years, there have been numerous reports in the media about potential risks of tests that use ionizing radiation. However, benefit-risk discussions about ionizing radiation from medical imaging are rare and seldom initiated by clinicians.For the new study, researchers from Memorial Sloan Kettering Cancer Center (MSKCC) in New York City analyzed over nine hours of transcribed conversations with 30 people who had undergone medical imaging exams to determine their understanding of the benefits and risks associated with various medical imaging procedures and their expectations regarding communication of those benefits and risks.
A substantial gap exists between patient expectations and current practices for providing information about medical imaging tests that use radiation, according to a new study published online in the journal Radiology. Researchers said the findings highlight a need for better communication as medicine enters an era of patient-centered care.In recent years, there have been numerous reports in the media about potential risks of tests that use ionizing radiation. However, benefit-risk discussions about ionizing radiation from medical imaging are rare and seldom initiated by clinicians.For the new study, researchers from Memorial Sloan Kettering Cancer Center (MSKCC) in New York City analyzed over nine hours of transcribed conversations with 30 people who had undergone medical imaging exams to determine their understanding of the benefits and risks associated with various medical imaging procedures and their expectations regarding communication of those benefits and risks.